Robert Wood Johnson Foundation New Connections regional conference hosted by USF
Robert Wood Johnson Foundation New Connections regional conference hosted by USF
Investing in young scholars who are underrepresented minorities (URM) is not only important for society and academia – it makes good business sense.
That theme was echoed by several speakers participating Feb. 27 in a regional conference sponsored by the Robert Wood Johnson Foundation (RWJF) New Connections national career development program and the University of South Florida. The day-long conference, titled “Uncovering the Institutional Impact of Scholars from Historically Underrepresented Backgrounds,” was held at the USF Marshall Student Center.

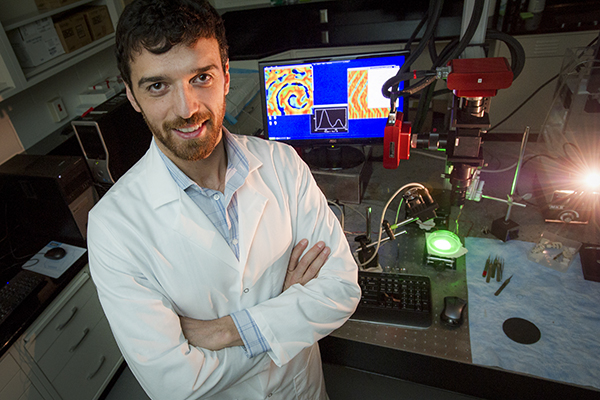
Members of the conference planning committee include, from left: June Lake, MA, USF College of Public Health; Devona Foster Pierre, EdD, assistant director of faculty/staff diversity at USF; Angie Harris, USF College of Public Health; and event co-chair Jacqueline Wiltshire, PhD, assistant professor in the USF College of Public Health who has been a New Connections scholar.
Participants came from five Southeastern states – Florida, Alabama, Kentucky, Louisiana and South Carolina – to define policies and best practices to help junior faculty and postdoctoral scholars from disadvantaged or underrepresented backgrounds advance their academic careers. Representing a range of disciplines and institutions, they discussed working towards breaking down the barriers that may prevent talented URM researchers from securing grant funding, a disparity documented in part by a study commissioned by the National Institutes of Health and reported in Science.
USF System President Judy Genshaft kicked off the conference by recognizing Jacqueline Wiltshire, PhD, an assistant professor in the USF College of Public Health and New Connections grantee who worked with RWJF to bring the conference to USF. Dr. Wiltshire’s recent research evaluating factors that may influence medical debt incurred by African American and white older adults was published in the American Journal of Public Health.

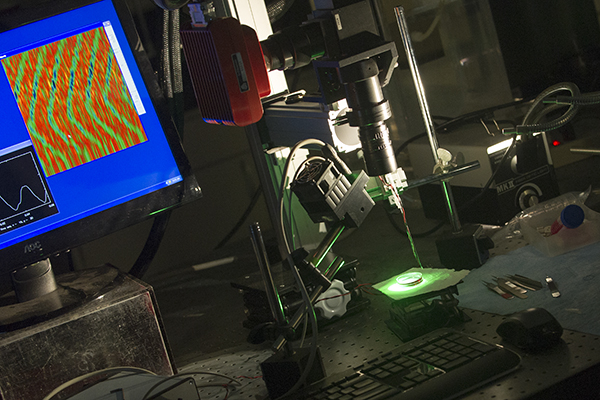
USF Health leaders shared their experiences and insights in a panel discussion framing how to move beyond numbers to best practices in supporting underrepresented minority scholars.
USF is proud of its diversity and will continue to seek even more diversity in student, faculty and staff recruitment, Genshaft said. “We look forward to continuing the conversation regarding underrepresentation on our campuses and in our workforce, and on making a positive and thoughtful impact on changing the face of the nation.
“I really believe universities are vital for advancing science and opening up people’s minds (to new perspectives), and diversity enriches education in every way possible,” she said. “This is especially true for health care and health research professions, who are caring for our ever-growing, more diverse population and discovering cures for our most complicated diseases.”
Role of university leadership in strengthening diversity
The plenary panel discussion “Diversity by the Numbers: The Role of University Leadership” featured four senior health leaders at USF. The panel fielded questions from Tyra Dark, a New Connections grantee and faculty member at Florida State University College of Medicine, and the audience. Below is an edited sampling of some of their comments and advice to junior and aspiring faculty in the audience:
Kevin Sneed, PharmD, senior associate vice president of USF Health and dean of the USF College of Pharmacy
Casting a wider net to find and recruit talented URM students and young faculty is just the beginning: “You can’t be a catch and release program… We have to make sure we’re bringing people along and providing them with continual mentorship. In my experience, if we’re not creating that level of sustainable relationship building, the influence of other areas very often will become a distraction to their pathway to (academic) success.”
Creating an environment to build trust: “I’m very fortunate that I’ve encountered an environment here at USF, starting with President Genshaft and vice president for health Dr. Lockwood, that is very collaborative and has allowed me to be me … You have to build an environment that is very welcoming to underrepresented minorities, that allows faculty to have very open and honest conversations (with leadership) about a whole host of things.”
Additional financial pressures often confronted by underrepresented minorities as they select career options, which can include higher-paying private sector jobs: “We have to work harder to mentor them at younger stages in their careers, all the way back to when they are students and in residency training, and help them overcome the financial debt that many of our students must overcome to advance.”
Catherine Lynch, MD, associate vice president of faculty development and women’s health, and the first woman to be promoted to professor of obstetrics and gynecology at the USF Health Morsani College of Medicine
The need to be aware of “unconscious bias:” “There’s plenty of data that shows if you have several women on your short list, the likelihood of a woman becoming a finalist for a major position goes up… If you don’t have underrepresented minorities as faculty within your department, it’s hard for (physician) residents who are underrepresented to say ‘this is a place where I want to be.’”
Some advice for women on advancing a career: “You need to be strategic in the (academic) service that you do. Be on the committee that’s going to help you advance and meet the right people — that will be the most valuable use of your time… If there are 10 requirements listed for a position, women tend to say ‘I don’t have number 7’ … But, if you already know everything on that list, you need to be looking for a position the next level up. Don’t assume if you work hard and keep your nose to the grindstone, you’ll be recognized for your efforts. Go to your supervisor and ask ‘what do I need to do to be the assistant director of so and so?’”
Edmund Funai, MD, chief operating officer for USF Health and senior vice president for strategic development at USF
Importance of leaving a legacy of people: “As university leaders we really have to be mindful of looking for talent everywhere and developing that talent. Talent isn’t necessarily right under your nose; you have to go a little further and look in nontraditional places.”
Advocating the business case for more URM representation in academia. “Part of the answer is… make the business case for diversity… And the business case for diversity, well known in the management literature, is that homogeneous groups do not produce as elegant or inclusive solutions as when everyone is represented around the table.”
Advice he gives all junior faculty regardless of their backgrounds: “When someone gives you something to do, do it a little better than they expect it to be done, but more importantly do it a lot quicker than they expect. Because when you’re talking about the hierarchy of departments and chairs, if someone delegates something and then they have to worry about it and ask you how is it coming, and they need updates, you’ve already failed… Your reward for that will be more work, but that’s the sort of behavior upon which careers are built.”
Donna Petersen, ScD, associate vice president of USF Health, dean of the USF College of Public Health, and interim dean of the USF College of Nursing
The role of faculty in preparing a pipeline of young scholars: “We have to reach back and commit to identifying young people and helping them get on a path so that they are not only prepared to join the academy, but want to join the academy… In both the (USF) Colleges of Public Health and Nursing, the numbers (of URM) are increasing, particularly in the assistant professor ranks where you have to start. In the nursing college, we have the additional challenge of needing more men in our faculty… and I’m very proud that our college of nursing actually has more male faculty than the national average.”
The importance of listening and meaningful dialogue to building a foundation of diversity in academia: “We can talk about numbers, but what’ are the stories behind the statistics?…Nothing is more heartbreaking than hearing the stories of underrepresented minorities who make it through layers upon layers of an MD or PhD program and then find themselves in an institution where perhaps they are the only ones who look like them.”
Health disparities research: “While we need more underrepresented minorities joining the research ranks to help us solve the problems of health disparities in this country, it’s not your burden alone to solve…I would say to URMs interested in pursuing higher education as a career, study whatever you want. You don’t have to study the things that are specific to the community you come from. If you want to, please do, but there are other ways you can engage in that conversation with the scholars focusing on health disparities.”

Jose Hernandez, EdD, associate vice president and chief diversity officer at USF, talked about what USF is doing to help scholars from historically underrepresented groups build the skills they need to succeed in academia.
Mentoring historically underrepresented faculty
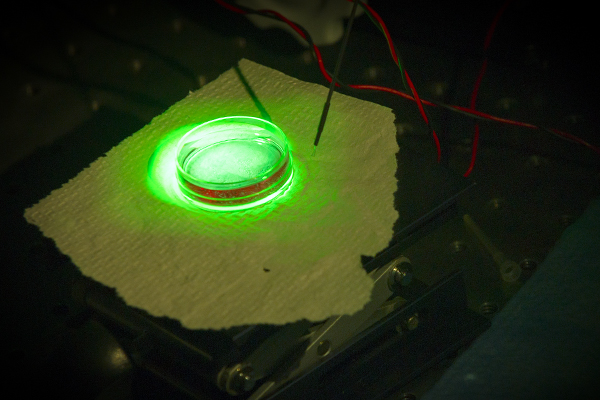
Another panel, which focused on mentoring historically underrepresented minority faculty, included Jose Hernandez, EdD, associate vice president and chief diversity officer at USF.
Dr. Hernandez, who immigrated at age 9 with his parents from Cuba to Puerto Rico, said that, for two years, he was the only Latino in his doctorate program at Florida State University. He helps mentor USF students in the McNair Scholars Program, which aims to increase graduate degrees awarded to students from underrepresented segments of society.
Dr. Hernandez spoke about USF’s Research Boot Camp© coordinated by the USF Office of Diversity, Inclusion and Equal Opportunity (DIEO), which he says was modeled after the research boot camp created by Sisters of the Academy Institute. Entering its third year, the USF camp offers an intensive one-week program in May designed to help women junior faculty, post-doctoral scholars and doctoral candidates, including women of color underrepresented in the academy, network with senior faculty and build the skills needed for success in academia. The one-week camp has been expanded to create a community of scholars with opportunities throughout the year to participate in sessions on research design and quality, publications, grantsmanship, and to discuss issues related to retention, promotion and tenure, he said.

USF’s Hernandez and other panelists listen to Bertha Hildalgo, PhD, of the University of Alabama at Birmingham, speak about how, with the help of RWJF New Connections grant funding, she developed her research investigating health disparities in cardiometabolic diseases. Her studies have focused on epigenetics in Latino populations.
USF also hosts a series of “Courageous Conversations” to help promote a culture of diversity and inclusion, Dr. Hernandez said, and best hiring practices workshops for faculty serving on search committees address the topic of implicit bias and how to mitigate it.
“We’re making a difference, but how can we do more? And how can you inspire us to do more, particularly with underrepresented minorities?” said Dr. Hernandez, who serves on the National Association of Chief Diversity Officers Board of Directors.
The RWJF New Connections program recently celebrated its 10th year supporting research grants and career development opportunities for a national network of more than 900 scholars from diverse, underrepresented and disadvantaged backgrounds. For more information, please visit http://www.rwjf-newconnections.org/.
Story by Anne DeLotto Baier and photos by Eric Younghans, USF Health Communications